Diabetes is a chronic condition that presents high glucose in the blood system. There are two types of diabetes: Type 1 diabetes is characterized by the body not producing enough insulin, and Type 2 diabetes is where the body cannot effectively use the available insulin. There is a global rise in the number of people living with complications of diabetes, cardiovascular diseases, kidney diseases, and visual problems.
Studies have shown a significant association of type 2 diabetes with individual lifestyle, aging population, and problems related to access to preventive and diagnostic services. For a quality life and reduced expenditure on treatment, we must focus on risk reduction.
In this post, you will learn:
Effective and proven approaches to managing your blood glucose through lifestyle and diet modification.
Available treatment options and transformed modern technology.
Barriers associated with the treatment and care of diabetes.
Why Diabetes Management Matters
Preventing complications
Prevention of diabetic complications is crucial to reduce further damage to the kidneys, nerves, and eyes. Also, it prevents heart attacks and strokes. These preventions make treatments more humane and less costly.
Improving life quality and longevity.
Risks of hospitalization can be reduced through the effective control of blood glucose. Ultimately, the symptoms will be managed, and general well-being and quality of life will be enhanced.
Reducing costs.
Management at an early stage lowers financial strain on individuals and the healthcare system. Long-term complications are often not easy to manage with diet and lifestyle modification or with treatment.
Recent guidelines by the American Diabetes Association Practice Committee emphasize timely intervention, use of technology, and a personalized care plan.
Section 2: Lifestyle Approaches to Diabetes Management
Physical activity
Studies have shown that regular exercise enhances insulin sensitivity by lowering blood sugar. Weight, which is also a risk factor, can be managed by physical activity. Significantly, the combination of proper diet and exercise has a better outcome. Studies have shown that glycemic index and metabolic markers can be improved more through a combination of a low-carbohydrate diet and exercise (Amerkamp et al., 2025).
Sleep and stress management
Research has indicated that insulin resistance can be worsened by poor sleep quality and chronic stress. The 2025 ADA report showed that type 2 diabetes can be improved by better sleep quality (3. Prevention or Delay of Diabetes and Associated Comorbidities: Standards of Care in Diabetes—2025 | Diabetes Care | American Diabetes Association, n.d.).
Weight management
The need for medication for type 2 diabetes can be achieved and maintained by maintaining a healthy weight. HbA1c, blood pressure, and lipid profile can be improved with weight loss between 5 -10%.
Diet for Diabetes
Evidence-based dietary patterns. Evidence has shown that the Mediterranean diet continues to show strong metabolic and cardiovascular benefits. This diet helps reduce HbA1c even when weight loss is modest (Barrea et al., 2025).
Plant-based diets also offer strong support for prevention and management by improving glucose control and lipid profiles and reducing cardiovascular risk.
Diabetes can be managed by other diets like low-carbohydrate, very-low-calorie, intermittent fasting, and limiting eating time. These diets have a proven control of glycemic index. Researchers are still looking at how this diet can be sustained and its long-term effects (Baskin & Karp, 2025).
Postprandial glucose spikes can be managed by the consumption of refined carbohydrates and maintaining a high-fiber diet in type 1 and type 2 diabetes. Most studies have shown that type 1 diabetes can be effectively managed by a high fiber diet and low carbohydrates (Zeng et al., 2025).
A medical nutritional therapy plan can be important to help an individual adjust macronutrient content, meal frequency, and the required energy for a patient’s lifestyle and metabolic status.
Treatment Options for Diabetes
Oral medications
The first-line treatment drug for type 1 diabetes is metformin. We also have newer classes of drugs like SGLT2 inhibitors and GLT-1 receptor agonists. Newer classes have additional benefits for cardiovascular and renal protection
Insulin therapy
Insulin therapy has improved the rapid and long-term management of both type 1 and Type 2. Some modern insulins, like glucose-sensitive insulin, can automatically adjust their activities depending on the current blood glucose levels. This trend has significantly improved insulin management.
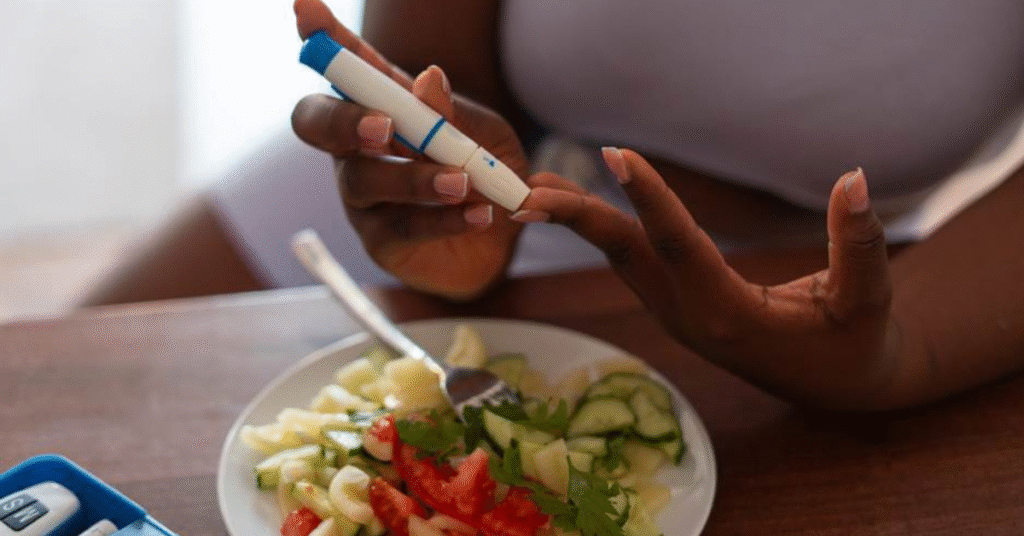
Smart pens/delivery devices
Insulin pens, continuous glucose monitoring devices, and automatic delivery devices have been introduced to reduce the dosage and monitoring burden.
Emerging technologies
Simulation tests (ABBA system) have demonstrated optimization of insulin dosing through reinforcement learning models. The rate of hypo- and hyperglycemia has been reduced by improving the interventional time (Akturk & American Diabetes Association Diabetes Technology Interest Group, 2024).
The Role of Technology in Diabetes Care
Continuous glucose monitoring (CGM) and automated insulin delivery (AID)
With these tools, real-time feedback is relayed in real time for timely interventions. AID can accurately regulate insulin administration depending on the feedback communication from the CGM. This has reduced the need for constant manual adjustments.
These tools give real-time or near-real-time feedback. AID systems adjust insulin based on
Apps and digital health
An advancement in modern mobile app technologies has led to a technological shift in diet monitoring, exercise and activity, drugs, and glucose levels. Most of these tools provide alert notifications, analyze trends, and provide telemedicine connectivity.
AI, predictive models, and near-future predictions
With these advanced technological features, CGM data can be predicted with a pinpoint level of accuracy, allowing swift planning and adjustments. That is possible because of the built-in sensors that can analyze trends depending on the stored and analyzed data.
Non-invasive monitoring research
Traditional invasive sample collection methods are often painful. There is advanced work that is exploring non-invasive modalities and sweat-based glucose sensors. There is a high correlation between the early models of glucose in research (Luo et al., 2025).
Barriers and Challenges in Diabetes Management
Access and cost
Advances in drugs, monitoring devices, insulin pens, and automated delivery systems are not fully covered by insurance; hence, they are very expensive for common people.
Sustainability of lifestyle changes
Evaluation of social, cultural, and financial factors is important. Sustainability of long-term goals may be difficult. It is not easy to always stick to special diets like low-carbohydrate, intermittent fasting, and low-calorie food over time.
Awareness and education
There are numerous misconceptions related to diet, stress, and the use of medications. It is not easy for patients and healthcare personnel to always understand the new diet options and the latest technology.
Health inequities
Some marginalized regions with low resources may lack access to testing, diagnostics, or care continuation. Also, the adoption of other modalities of treatment may be affected by cultural preferences and social structures.
The Future of Diabetes Management
Several factors must be individually considered. Studies suggest a combination of genetics, microbiome evaluation, and metabolic reviews to prescribe diet and drug therapies.
A combination of telemedicine and remote monitoring with digital health devices has enhanced the proactive management of diabetes. Use of this tool has shown effectiveness in predicting periods of blood sugar instability.
Primary prevention and early management initiatives have increased. More weight is put on quality sleep and stress management (3. Prevention or Delay of Diabetes and Associated Comorbidities: Standards of Care in Diabetes—2025 | Diabetes Care | American Diabetes Association, n.d.).
FAQs
Q1. What is the best diet for diabetes management?
There is no single and specific diet for managing diabetes. Each available diet depends on individual preferences and health status, lifestyle, availability, and sustainability.
Q2. Can lifestyle changes reduce the need for medications?
It depends on timing. Regular screening and following preventive measures will significantly delay the need for medications. Diet and exercise can lower the HbA1c.
Q3. How effective are new technologies in diabetes care?
It is very promising. Automated delivery of insulin and predictive AI models are helping with the prediction of glycemic trends.
Summary
A combination of lifestyle, diet, and treatment is the key determinant for the effective management of diabetes. Mediterranean diets or plant-based diets with physical activity have a significant impact. New technologies have expanded options for the treatment and monitoring of diabetes. Your health management matters. Enhance your healthy lifestyle with regular checkups and explore newer technological tools that ease the monitoring and treatment burden.
References
3. Prevention or Delay of Diabetes and Associated Comorbidities: Standards of Care in Diabetes—2025 | Diabetes Care | American Diabetes Association. (n.d.). Retrieved September 16, 2025, from https://diabetesjournals.org/care/article/48/Supplement_1/S50/157550/3-Prevention-or-Delay-of-Diabetes-and-Associated?utm_source=chatgpt.com
Akturk, H. K. & American Diabetes Association Diabetes Technology Interest Group. (2024). Recent Advances in Diabetes Technology and Activities of the American Diabetes Association Diabetes Technology Interest Group. Clinical Diabetes, 42(2), 316–321. https://doi.org/10.2337/cd23-0080
American Diabetes Association Professional Practice Committee. (2024). Summary of Revisions: Standards of Care in Diabetes—2025. Diabetes Care, 48(Supplement_1), S6–S13. https://doi.org/10.2337/dc25-SREV
Amerkamp, J., Benli, S., Isenmann, E., & Brinkmann, C. (2025). Optimizing the lifestyle of patients with type 2 diabetes mellitus—Systematic review on the effects of combined diet-and-exercise interventions. Nutrition, Metabolism, and Cardiovascular Diseases: NMCD, 35(5), 103746. https://doi.org/10.1016/j.numecd.2024.09.016
Barrea, L., Verde, L., Colao, A., Mandarino, L. J., & Muscogiuri, G. (2025). Medical nutrition therapy for the management of type 2 diabetes mellitus. Nature Reviews. Endocrinology. https://doi.org/10.1038/s41574-025-01161-5
Baskin, R. G., & Karp, K. A. (2025). Navigating the Spectrum of 4 Evidence-Based Nutrition Options for Type 2 Diabetes Management. The Journal of Clinical Endocrinology and Metabolism, 110(Supplement_2), S112–S117. https://doi.org/10.1210/clinem/dgae646
Luo, J., Kumbara, A., Shomali, M., Han, R., Iyer, A., Agarwal, R., & Gao, G. (2025). A Large Sensor Foundation Model Pretrained on Continuous Glucose Monitor Data for Diabetes Management (No. arXiv:2412.09727). arXiv. https://doi.org/10.48550/arXiv.2412.09727
Zeng, J., Beck, M., Barouti, A. A., Löfvenborg, J. E., Carlsson, S., & Lampousi, A.-M. (2025). Effects of different dietary patterns on glucose management in type 1 diabetes: A systematic review and meta-analysis of randomized controlled trials. EClinicalMedicine, 83, 103222. https://doi.org/10.1016/j.eclinm.2025.103222